Scoliosis and Osteoporosis
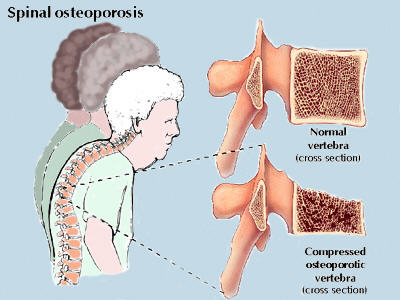
A concern with degenerative or adult-onset scoliosis is how it is affected by osteoporosis. Osteoporosis and scoliosis are related because they are both conditions which affect the spine. Osteoporosis is a disease that affects the density or mass of bone structures. Millions are diagnosed with the condition, which decreases the strength of bone and may lead to reduced protection against fractures. It is accompanied by brittle and/or porous bones and is associated with loss of bone-building nutrients such as calcium, vitamin D and magnesium.
Osteoporosis by itself isn’t associated with pain but compression fractures that may result because of it can be very painful. About 15-20 million people have osteoporosis, and over half a million suffer spinal fractures due to osteoporosis each year. These fractures can occur in scoliosis patients on the concave or convex side of their curvature. It is not known whether or not osteoporosis causes scoliosis but it does cause kyphosis a rounded or humped back.
Risk Factors
Women are at a greater risk of developing osteoporosis because they generally have less bone mass than men. Also, hormonal changes that take place during menopause can deplete bone density and women tend to live longer than men. Though women are at greater risk, roughly 2 million men in the U.S. have osteoporosis and another 3 million are at risk.
Another risk factor is race. Asian and Caucasian women who are small boned, are at highest risk for osteoporosis. Similarly, there is a greater tendency for Adolescent Idiopathic scoliosis patients to be slender women. So much so that studies [1,2] have suggested a possible link between scoliosis and osteoporosis. One study states that osteopenia (bone density that is lower than normal) is common among AIS patients and “The prevalence of osteoporosis in AIS patients is much higher than in the general pediatric and adolescent population” [1].
Like adolescent idiopathic scoliosis, genetics are another contributing factor for developing osteoporosis. Like scoliosis, osteoporosis runs in families. Though family history increases your risk of developing the condition, it does not mean you WILL develop it. In fact, one study compared body mass index (BMI) and bone mass density (BMD) of AIS patients to that of their siblings. The study found that not only did the patients with scoliosis have lower BMIs but they also had lower bone masses than their siblings with normal spines [2]. This further suggests a connection between the two disorders. What this connection is, is still to be determined. Does scoliosis cause osteoporosis? Does osteoporosis cause scoliosis?
Certain lifestyle choices have also been linked to osteoporosis. Poor diet, smoking, excessive consumption of alcohol, and inactivity can all increase your risk. Certain metabolic disorders can also contribute to osteoporosis such as Cushing’s syndrome, hyperthyroidism, and hyperparathyroidism. As well as certain gastrointestinal disorders that can affect the body’s ability to absorb calcium.
Prevention
After the age of 18, all women (particularly postmenopausal women) are advised to take 1500 milligrams of calcium per day along with the amount of vitamin D found in a multi-vitamin. Additionally, in the first five years after menopause, it is suggested that women take the hormones estrogen and progesterone–provided they have no history of breast cancer or uterine cancer. Then, after five years, women are advised to stop hormone treatment and continue taking the vitamin D and calcium combination. Staying in shape through moderate exercise is also advisable for prevention of many conditions and diseases.
With osteoporosis and adult scoliosis precaution must be observed before exercising. These conditions offer different challenges depending on age, severity and prognosis. It is best to discuss with a scoliosis exercise specialist which types of exercise are best for your specific case and which should be avoided. Specialized exercise programs for adult scoliosis patients are based on exam and xray results.
Exercises that maintains or increases flexibility may be beneficial if you’ve been diagnosed with osteoporosis and scoliosis. Low-impact and gentle stretching and toning exercises such as yoga, Pilates and tai chi, may reduce pain and limited range of motion caused by either condition. Walking is another low-impact weight-bearing exercise that helps maintain flexibility, strength and stamina.
Stretching exercises can also help maintain strength and stability for those diagnosed with scoliosis and osteoporosis. Abdominal stretches as well as back and hip stretching exercises may help increase flexibility. Stretch the hamstrings, which are the muscles along the back of the thigh, the quadriceps, or thigh muscles, and the hip flexors, found at the hip joint, on a daily basis.
Cautions
If you’ve been diagnosed with low bone mass or osteoporosis, talk to your scoliosis doctor about safe exercises that won’t worsen your condition or cause further injury to bones and joints. Avoid high-impact exercises that severely affect the bones and joints.
Back pain is the most common symptom of this condition, and x-rays may show wedge or compression fractures of the vertebrae. It is very important to confirm a diagnosis of osteoporosis as symptoms occur with other conditions such as infections, other metabolic bone diseases, and benign or malignant bone tumors. The extent of the osteoporosis can only be estimated on X-rays and must be confirmed by specific bone density tests or, in some cases, by bone biopsy.
Visit the National Osteoporosis Foundation website for more information on osteoporosis and treatment.


